As organizations increasingly recognize the power of virtual care, more providers are turning to remote patient monitoring to help them strengthen the provider-patient relationship and change how people access healthcare. Through remote patient monitoring platforms, patients can be monitored from the comfort of their homes via wearables, IoT devices, and sensors, thus eliminating unnecessary patient visits and improving patient engagement & self-management. Curious to learn more? Here’s a quick reference guide that covers what you need to know about remote patient monitoring.
Table of Contents
GENERAL FAQ
What is a remote patient monitoring device?
Is it better to buy or build a remote patient monitoring device?
How long does it take to build An RPM solution?
How much does it cost to build an RPM app?
What is remote patient monitoring?
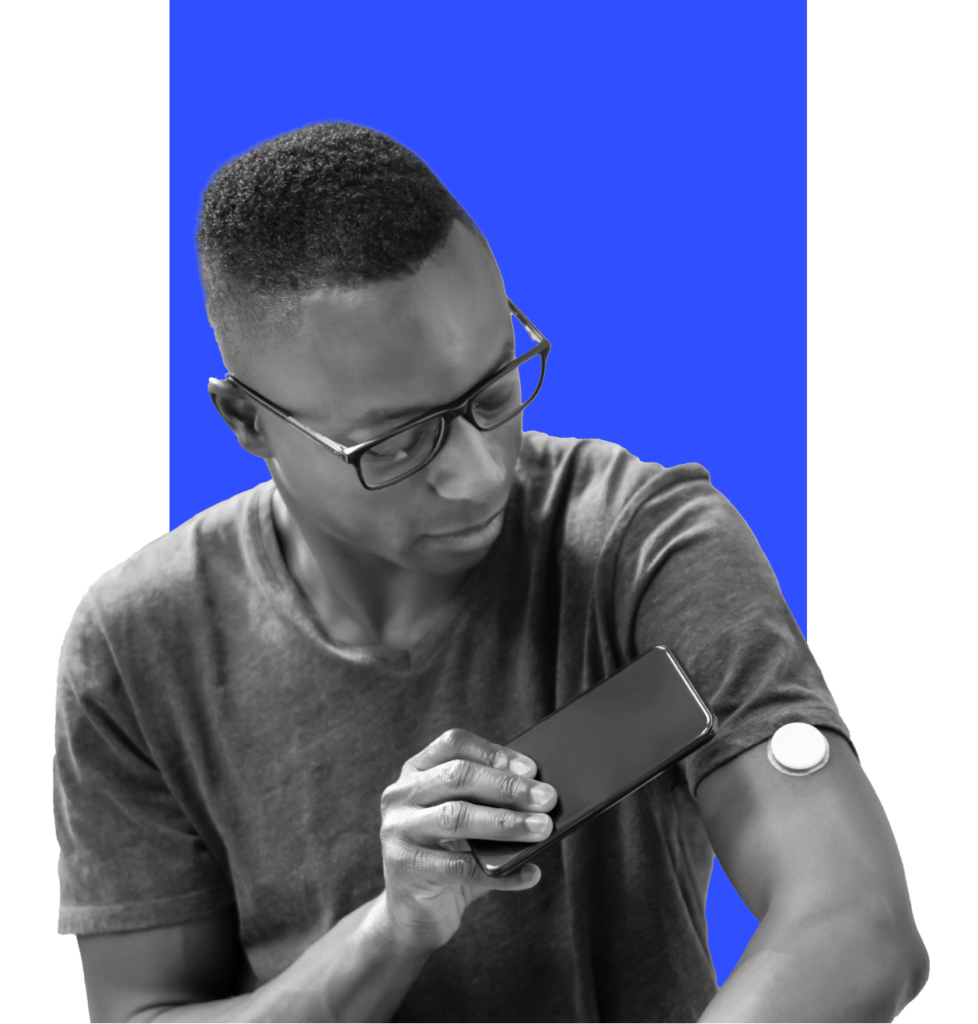
Remote patient monitoring (RPM) is a digital health solution that enables healthcare professionals to monitor and capture patients’ health data outside a traditional healthcare environment. Remote patient monitoring technologies collect and record patient data for review, diagnosis, and clinical management. New monitoring devices are emerging daily, but a few common examples include blood pressure monitors, cardiac implants, and blood glucose meters. Below are a few stats that demonstrate RPM’s emerging role in healthcare.
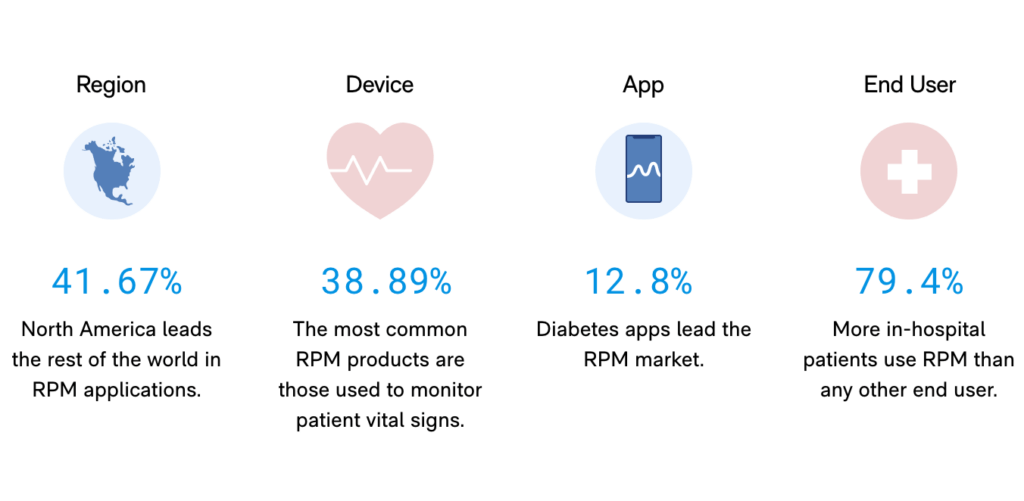
RPM by the numbers
The global remote patient monitoring market is projected to triple to $175 billion by 2027. Some key factors driving this growth are the rising number of chronic diseases, a growing geriatric population, and advancements in telecommunications.
*Source: Strategic Market Research LLP
RPM statistics
Benefits of Remote Patient Monitoring?
Accelerated by the pandemic, RPM has proved to be one of the most significant drivers in reshaping the Health at Home model. Now widely accepted by hospitals and health systems worldwide, RPM offers convenience to consumers while reducing time spent in high-cost settings like hospitals and assisted living.
Key benefits of Remote Patient Monitoring

- Extends & improves access to care
- Improves outcomes through earlier symptom detection
- Enhances patient engagement & self-management
- Strengthens the patient-clinician relationship
- Improves data-driven decision-making & clinical insights
- Reduces hospital-acquired infections
- Improves clinician satisfaction
- Promotes better access to care
- Eliminates unnecessary patient visits
- Reduces missed appointments
- Increases the efficiency of nurses and providers
- Boosts net patient revenue
- Better utilizes medical resources
- Reduces hospital re-admissions
- Contains administrative costs
- Lowers cost of care for payers & providers
How remote patient monitoring works
RPM enables patients with chronic or recurring conditions to receive continuous monitoring and treatment outside a clinical setting. This allows clinicians to collect patient data in real-time, thus reducing the need for routine in-patient visits while strengthening the patient-clinician relationship. See the use case below to learn how a diabetes patient can better manage their care using an RPM app.
Remote Patient Monitoring use case
Michelle has Type 2 diabetes and needs round-the-clock monitoring of her blood glucose levels.
A physician-led care team provides Michelle with a connected glucometer that allows for the automatic wireless transmission of blood glucose readings to the team. The team also gives Michelle a mobile app to help track her blood sugar and other health indicators. Michelle can view her care plan, log food intake, order test strips, and receive health coaching through the app. Michelle is instructed to self-test her blood glucose daily. A care team member reviews the transmitted readings and follows up with Michelle if her results show a deterioration in glycemic control. The care team also provides Michelle with ongoing coaching through the app.
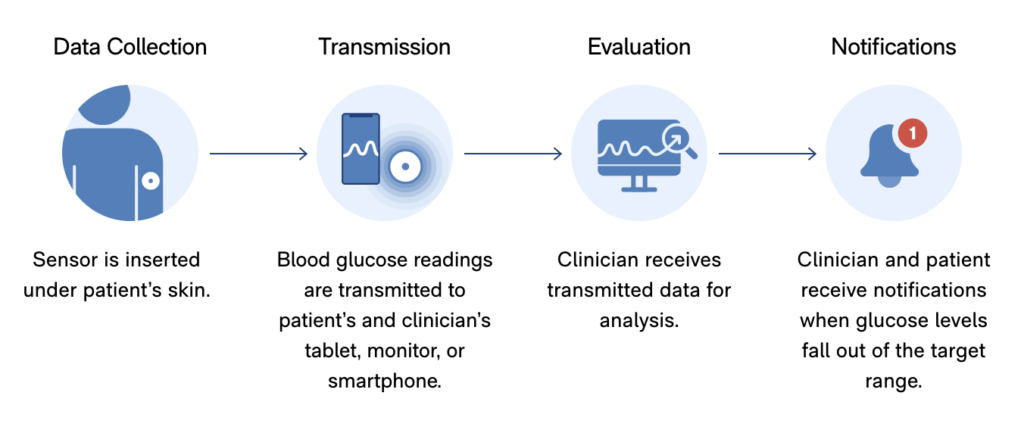
Every month, the RPM vendor sends a report to Michelle’s primary care provider with an update on her glycemic control and condition. In addition to the monthly reports, the vendor contacts Michelle’s primary care provider if any other health issues arise.
Michelle’s RPM solution helps reduce her need for in-person visits and promotes early intervention by clinicians who track her data digitally. Through easier access to diabetes care management, Michelle can better maintain healthy blood sugar levels and improve her overall health outcome.
15 steps to RPM implementation
As more organizations discover how RPM can transform care delivery and improve patient outcomes, many are making RPM a strategic priority. Not sure where to start? Here are 15 quick steps to guide you through RPM planning and implementation.
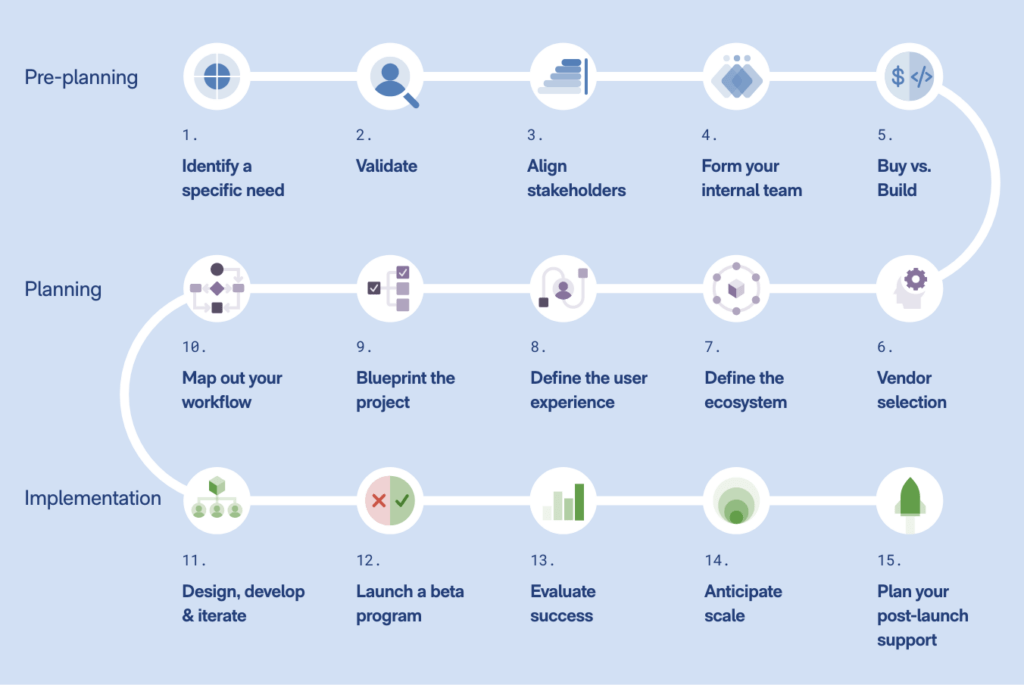
Pre-planning phase
1. Identify a specific need and desired outcome
What challenges are you facing as an organization? What patient needs are not being met today that could be improved with RPM in place? RPM can be used to track a wide range of conditions, including heart disease, diabetes, asthma, and Parkinson’s. Your frontline staff can help you identify the pain points and opportunities RPM can most effectively address in the day-to-day needs of patients and clinicians.

2. Validate your product with real users
Are you taking a patient- and provider-centric approach when considering your RPM solution? Get to know your users’ needs, pain points, and desired outcomes through a systematic approach to user research.

3. Align stakeholders
Are your teams aligned on process and intended outcomes? Successful RPM implementation needs executive buy-in and commitment across departments, including clinician, administrative, and IT teams.
4. Form your internal team
Have you identified key individuals to lead? Implementing an RPM system requires an organization-wide commitment and a leadership team comprised of individuals from each department who will touch the RPM system. Recruit your most innovative thinkers to lead the initiative.
5. Evaluate ‘buy vs build’ scenarios
What are the pros and cons of buying or building an RPM system? Health professionals are overwhelmed by countless digital products that have failed to address the specific needs of patients and providers. Evaluate the pros and cons of buying an off-the-shelf product vs. building a custom product.
Planning phase

6. Vendor selection
Have you considered your team’s capabilities and time capacity for your initiative? Internal IT typically does not have the same skill-sets as a product, design, and custom software development company, yet it will be a key partner in integrations, security, and compliance. Also, evaluate the pros and cons of using a vendor with onshore vs. offshore resources.
7. Define the ecosystem
How will you set up a secure RPM ecosystem? Your internal IT team will be a critical stakeholder in signing off on your implementation. You’ll need a full stack of technologies, including Bluetooth connectivity, a mobile interface, a server for data transfer, and secure data storage. In addition, the ecosystem must be reliable & fault-tolerant, with continuous device functionality with or without an internet connection.

8. Define the user experience
How well do you understand your user’s journey? A frictionless user experience is critical to user adoption. You’ll need an intuitive interface specific to your users and their conditions. For example, can your patient operate the device and system on their own without the help of vendor training?
9. Blueprint a process
Who will help you outline each step in the implementation process? When considering an RPM system, you’ll need an experienced partner to outline each step, from identifying technology requirements to planning for scale.
10. Map out your workflow & integration needs
How will RPM integrate into your practice and network? Establishing a workflow across departments can help you identify integration points and ensure system continuity. In addition, you’ll need to implement privacy and security controls throughout the ecosystem to safeguard patient data and prevent medical identity theft.
Implementation phase

11. Design, develop and iterate
Product acceptance is critical to getting your program off the ground. A strong product, design, and development team can ensure that the right product is built for the right end users. The more upfront effort you put into validating the correct experience, the faster you will get to market with high quality.
12. Launch a beta program
Have you considered a beta program to test your system with real users? Launching a beta program is one of the most effective ways to gather user feedback and fix any bugs before a final release. Work with your vendor to set up a training program and quick-reference guides for your staff and patients. Proper training will ensure user adoption
13. Evaluate success
How will you measure patient engagement? By defining goals on the front end, you can track program success and communicate findings to your internal stakeholders.
14. Anticipate scale
Do you have the resources and infrastructure to scale your program? In the planning stage, anticipate what you’ll need for future growth.
15. Plan for post-implementation support
Have you considered all your post-launch support needs? Post-launch support is critical to the ongoing functionality and security of RPM systems. Ensure that you have support staff who can provide ongoing software maintenance and are fully trained in HIPAA compliance.
The future of RPM
Remote patient monitoring is transforming healthcare. Now one of the most effective tools used to treat chronic and acute conditions, RPM has entered the mainstream as a powerful solution that can provide more timely and efficient care. As healthcare providers continue to harness the power of RPM, new healthcare applications will proliferate – along with more ways to deliver high-quality care that will improve the patient experience.
Let us help you start your RPM journey today!
Remote Patient Monitoring FAQs
Is telehealth the same as RPM?
Not quite. Telehealth refers to an industry that uses telecommunication as a way for healthcare providers to care for patients remotely, without an in-person visit. The most common example of telehealth is video conferencing.
RPM is a subset of telehealth. RPM specifically refers to the practice of monitoring and capturing patients’ health data outside a typical healthcare setting using wearables, IoT devices, and sensors.
What are the most common devices used for remote patient monitoring?
New RPM devices are being developed each day, but the most common type of device currently used is a smartwatch, blood pressure monitor, blood glucose monitor, pulse oximeter, smart scale, spirometer, and medical alert system.
What diseases can be managed using RPM devices?
Many chronic conditions can be monitored using RPM systems, and the list is growing. Among the diseases that are often managed using RPM devices are hypertension, diabetes, congestive heart failure, COPD, hypertension, pneumonia, and post-surgical cases.
Who can use RPM?
With the expansion of telehealth during the COVID-19 crisis, more patients than ever can now have access to healthcare through RPM devices. In 2021, the Center for Medicaid and Medicare Services (CMS) issued a final rule that practitioners may provide RPM services to remotely collect and analyze physiologic data from established patients if the monitoring is reasonable, medically necessary, and “used to develop and manage a treatment plan related to a chronic and/or acute health illness or condition.”