This transcription is provided by artificial intelligence.
Today on This Week Health.
Do you want to be informed or influenced? But big parts of America don’t want to know. It’s a lot just to step on the scale. A lot of the hospital organizations are dealing with, part of the population that’s In denial Welcome to Newsday -This Week’s Health Newsroom Show. My name is Bill Russell. I’m a former CIO for a 16-hospital system and creator of This Week Health, A set of channels dedicated to keeping health IT staff current and engaged. For five years we’ve been making podcasts that amplify great thinking to propel healthcare forward.
Special thanks to our Newsday show partners and we have a lot of ’em this year, which I am really excited about. Cedar Sinai Accelerator. Clearsense, CrowdStrike,. Digital Scientists, Optimum Healthcare IT, Pure Storage, SureTest, Tausight,, Lumeon and VMware. We appreciate them investing in our mission to develop the next generation of health leaders.
Now onto the show.
All right. Here we are. It’s another news day, and I’m joined by Bob Klein with Digital Scientists. Bob, it’s always great to catch up with you. There’s a lot going on in the world of health care and AI. These days. So I think we’re going to hit on some of those stories that surprise you that we’re talking about I hear at the end of 2023.
No, there’s really nowhere. Nowhere to run. It sometimes just feels like a chance for us to put on our analytics hat. You know how to make sense of all that data that’s out there.
There’s a lot of positive stories. There’s a Stanford story. Just a couple of other things we talked about.
I want to start with this question. 3 and 4 Americans who believe AI is going to reduce the number of jobs, reduce the number of probably white collar jobs and jobs. You’ve been playing with it. I’ve been playing with it. Does that ring true to you that there’s going to be a reduction in the number of jobs?
I’m sure there’s a positive spin on this, but that’s the Gallup poll that’s out there.
Well, I think there’s, the jobs are definitely going to change. Right. And I don’t think it’s a zero-sum game for jobs. I think there will be, new kinds of jobs. I mean, new ways that we’re going to have to leverage it.
But it’s hard for me to say it will likely cause some dislocation and in a way I look at AI as bringing computing power to bear where it’s been hard to access, right? So sometimes in healthcare, you think that the only computing power is walking on two legs and has an MD, right?
So there’s a lot of computing power that’s out there that hasn’t been really brought to bear. But think it’s not going to be a replacement anytime soon for kind of high-touch interactions or for highly skilled, highly creative those kinds of areas and hopefully it’ll be freeing for people to focus on things where they can really excel, get rid of some of the drudgery – the data entry and things like that we really shouldn’t be doing.
Yeah. And that’s what I’ve been talking to people about. If you’re worried about your job specifically, it’s not stop focusing on the outcome of your job. Start focusing on how you do your job, right? So the way we interact with people, the way we rally people around a cause, the way we
Are we able to move problems through, there’s still an awful lot of things that AI in its current form is not anywhere near. And it’s that ability to rally people to, tell a story to bring things together. That’s one of the things I’m talking about, but the thing that I’m finding really fascinating.
Is the pace at which we are moving from AI being the purview of technologists to AI being the purview of the everyday physician or clinician or those kind of things. I’m looking at the new GPT stuff, so chat GPT, they have their keynote and they have these new things, GPTs, which are apps.
But essentially you could. It’s not a programming language. It’s just you in front of a computer with natural language saying, hey, I’d like to create this thing that has this special knowledge base. Oh, by the way, here’s these PDFs that have this special knowledge base and some other things.
And all of a sudden you’ve created this specialized GPT, which is what they call a specialized GPT. And I created one called Health System CIO. And I put a bunch of our, conversations and interviews and that kind of stuff. And I put all that stuff in there. And then I asked it a basic question like I’m thinking about doing an EHR implementation.
What’s the best process? And it spits stuff back to me. I’m like, That’s really good. It’s not like the computer is that smart. It’s just, that it’s pulling from this wealth of information that me without any programming just dumped into it.
I mean, I do think it’s going to be highly accessible and that’s why I was saying, it’s analytics and access, like how to make sense out of so much data.
Honestly, a lot of the data we get and very much so in healthcare. There’s no time or energy or none of people writing SQL queries. I mean, oh, my gosh, totally transactional. Like I said, for us to create data models for an individual or patient level, it’s going to take so much effort. And.
It’s going to be, it’s going to make it easier to do that. Right. And all the disparate data sources. It just feels like, this computing power is going to be available. And like you said, we’ve got, tools to make it easier for everyone. It’s not the purview of I. T. And honestly, a lot of times.
IT is too busy, keeping the network up and running and dealing with other kinds of security and, they’re dealing with a lot of other tasks. They would love to probably spend more of their time in this area. But a lot of times they don’t they just can’t, so it’s got to be made accessible and there used to be something called if this than that, or something like that, plug and play, you.
Precursor to plugins and stuff like that. But I think we’ve we’ve learned a lot in that area and we need people to experiment. I mean, basic clustering algorithms just again, it’s making sense of the data and even sometimes it’s just access. Question and answer.
I had somebody that was working on something around HSAs, trying to educate people about HSAs. You think, how much is there to educate about HSAs? But apparently, most people don’t know that it’s a decent investment vehicle and all this other jazz, but it’s all trapped in a book. It’s like, well, we want to be able to facilitate Q&A; against knowledgeable or qualified data sources.
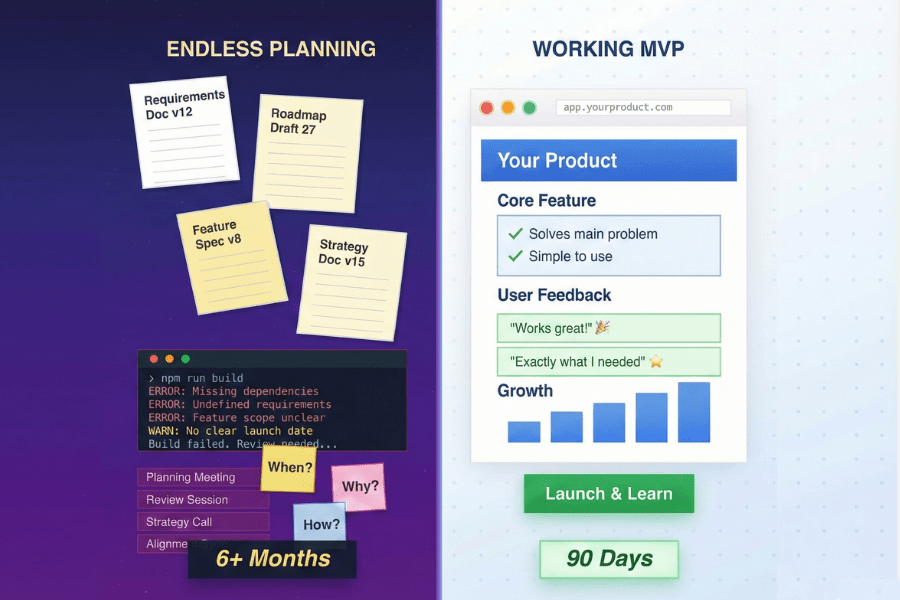
So it’s. And it’s just what you have put together. So it’s gone really far in a single year. Never mind all the politics and the theatrics open AI just recently, but that’s still has a lot of promise. I guess the question for you is, I don’t know if health IT or the folks inside health organizations are going to have the wherewithal to actually create some of their own models, right, to create some of their own because I don’t see necessarily the funding, the training source, the resources internally, and the bandwidth to be able 📍 to do it , or enough training data, I would say.
I think it’s the bandwidth. Yeah. because this is so accessible to the everyday person within the healthcare organization. And they can start playing around with it recently, I was going back and forth with kids, literally like 16, 17-year-old kids who are training these models.
I’m going, oh, my gosh, like, now I know what it felt like when I came out of. College and I knew how to use a computer and the next generation was looking at me going, Oh my gosh, this kid wants to use a computer for this stuff. What is he thinking? That’s how I sort of look at these kids now are coming out and going, Hey, I trained my own model on this thing.
But I agree with you. I think there are some limitations in terms of really understanding the data that you do have and preparing that data. to be used by these models. But I think it’s the bandwidth that’s really going to slow us down. And that actually gets us to the first story is Stanford Health.
Uses AI to reduce clinical deterioration events. I think this is going to be a common headline next year. This is clinical deterioration events and for chronic conditions and those kinds of things. And it’s keeping an eye on the telemetry data and it’s using AI.
By the way, telemetry data is some of the cleanest data we have in healthcare. Cause it’s just. It’s a lot of data points, time series over a period of time, followed by things being logged in the EHR that say, hey, this happened, or this happened, or this led to an adverse event. And so we just have tons of this information.
It’s fairly clean, and it’s not surprising. that this is one of the use cases, but Stanford’s probably, to your point, Stanford has the resources, it has all of those things. And it’s important to note that I don’t, I don’t see Mike Pfeffer’s name anywhere in this article.
This is. This is some people within Stanford who are a practicing academic internist, a board certified practitioner. They’re leaning on some of the resources that Stanford has, but they’re not going to the IT department saying, Hey, I’ve I’ve got some ideas or some thoughts here.
And they might even tap into a third party or somebody else and bring them in and say, Hey, look. We have this concept for those who don’t have the resources and don’t have the bandwidth, think you’re going to need to keep up on this stuff. And I think tapping into those third parties, it’s going to be one of the ways you do it.
Do you think IT’s RPM finds its way into the hospital? So that mindset of everyone there actually in the organs, if you’re in a hospital bed, everything is being logged, everything is going into the EHR, at least there’s not this kind of lag, whereas if you’re, I almost think of it as like an RPM hub it’s very much of an outside-in thought process where there’s, inside of health IT, there’s always this process.
The idea of like, well, if it’s not in the EHR, it’s not real, or we don’t know what the hell to do with it. Right, but there’s, if you’re doing health at home, like, they’ve had to create this infrastructure outside of the EHR, or on top of it, where I’ve got all this physiological data, and I’ve got a hub it has to come to, I have to create a model to understand it, and I have, but I have the real-time access, and I can make real-time decisions.
Based on trending data, and it’s just that same model back inside the hospital.
Let me ask you this, remote patient monitoring, the data from a remote patient monitoring, which by the way, I’ve talked to physicians for years, and they just don’t want it. I mean, they want the clinically approved devices.
It’s not in the EHR, right? Right, they just don’t want it in the EHR. They don’t want to be liable for it and all that other stuff, but is that not the data? That, Google collected early on, like, number of clicks, number of searches, number of this, number of that, don’t you think long term it’s short-sighted to not want that data and that information?
Cause that’s going to lead to. Sort of an, if you’re, stay with Stanford, if I’m Stanford and I’m collecting all that information for a hundred-mile radius from around my campus, does that not give me a competitive advantage of looking demographically and geographically, all this stuff and slicing and dicing it and then delivering care in a different way over the next five years?
I have to think that data is as valuable as the data Google was collecting early on in the internet.
Absolutely. You need it all. You need it all, and you can’t you’re not going to get any smarter about an individual patient, or a population without it. Just be, whether it’s in the EHR or not, it doesn’t matter, and, they don’t like it because they can’t make sense out of it, and they’re asked to make decisions on too much data.
So that’s some of, That’s the way it’s treated, but it’s not that it doesn’t have value, until they use AI, there’s not the ability to extract the value. It just becomes, onerous because it’s not in the format that the providers want to see it, which is in the EHR.
But it doesn’t mean it’s any less valuable, and there’s more data just makes it more of a challenge to analyze. I do think that that’s some of the promise of AI is helping make sense out of it, and honestly, for the things that we work in, there’s a lot of data, let’s just say medical coding, for example, right, so, to get involved in some of these things, we’ve got to make sense out of for value-based care and accountable care organization you’re really motivated for typically a smaller population to be very smart about that person’s comorbidities, everything they’re dealing with, to keep them out of the emergency room.
And if you don’t do a good job at that, and you’ve got probably two years of flames data, you’ve got all their kind of their interactional data, you’ve got all their EHR data. And it’s your job to assess them for what is it, a risk adjustment factor, right? A RAF score. So… As this ship slowly turns, if you don’t take all the data that’s available to you and make sense out of it for an individual patient and by extension of a population probably of a, of, some similarity, you will lose money and you could go out of business, right?
If you’re running an ACO, it won’t make it. And I’m talking more from experience dealing with the Medicare population and they need more tools needs to end up in the EHR, but not everything is epic, right? So, I’m talking about Point Click Care (PCC) and the EHRs, there’s still a lot of different ones that still have to make sense out of it, but I think that’s the challenge AI has to help people make better decisions.
It makes sense out of huge data sets that are just overwhelming at the moment.
I’m wondering who is in the best position to take advantage of this. The payer, provider is it tech? I mean, is it Apple? Because Apple has collected a ton of this information over the years. Is it Apple?
Is it Amazon as one of the tech players? And that leads to, today’s headline, Cigna and Humana in Talks to Merge. Okay,
Yeah. Well, I mean, my gosh these what, UnitedHealthcare is what, 250 billion a year or something like that.
Cigna, Humana combined. I’m going to get these numbers wrong, but it has to be over 100 billion. ’cause I, Cigna at one point I think was 50 to 60. Humana can’t be much smaller than that. So this is, had, has to be a hundred billion. And just when you thought consolidation was done in the carrier space to have this come down?
I think it’s a I think it’s a major story. I think it, it just keeps, continues to show that the payers have done really well. through this last four or five years healthcare providers financially have not done that well.
No, they’re, I mean, is this the path to single-payer?
Yeah, well, yeah, the path to single-payer is eventually to be honest with you, I’m shocked that from a regulatory standpoint, it just continues to consolidate at this pace and no one seems to throw up their hands and, was it Teddy Roosevelt?
Who was the buster back in the day, the union buster. I, or not union buster, the monopoly, yeah, yeah. Trust buster. That’s what it’s trust buster. Yeah. I mean, I’m just shocked. I mean, these things are huge and they have. Multiple arms going in a lot of different directions.
By the way, the other story that’s starting to really bubble up is the number of providers that are saying no to Medicare Advantage. It’s really interesting. I mean, they’re pushing back and saying, look, it’s working well for you, but it’s not working for us.
Why is that, Bill?
Why is that there? I mean, is it the I mean, all I’m always trying to figure out, because I’ve got that decision around, straight Medicare versus Medicare Advantage and all the kind of supposed benefits, but a limited network access, those trade-offs, like how to, it always feels like.
This answer is going to get me, I don’t know the numbers well enough to be intelligent on the space, but I will say this. There’s been a number of articles that have talked about the amount of fraud that is associated with Medicare Advantage because it’s the coding that gets them, additional dollars based on the government payouts because it’s around Medicare, right?
So it’s a federally funded, kind of program. And so if somebody has certain codes and certain things. then therefore they generate more dollars for the payer. And so there’s a push to do coding in a way that, I mean, at least if these articles are to be believed and the, quite frankly, lawsuits that are following them there’s a fair amount of coding that is questionable based on Medicare Advantage and reimbursements.
Isn’t that Medicare’s fault? Like, I mean, I’ve looked at this where, what defines the truth? It’s the truth is what Medicare is willing to pay for, and if it’s been fuzzy and Unclear then people will test it and then for Medicare advantage is like, how do I make more money?
Well, here’s my understanding So you present you come to me as the doctor and I look at you and I say well, you know This is what you have, but I’m gonna code it this way because this will get us more money I mean, is that Medicare’s fault or is that sort of trying to game the system? I mean, if it is what you have, then by all means, code it that way.
But if it’s not what you have, then we’re just playing games to get more money.
there have to be tests. There have to be, analysis of what’s in there for assessment. But the same, I mean, you don’t think something similar is going on with…
The Cigna’s and Humana’s? I mean, that was mostly denial.
We talked about this last time, was the auto denial from Sigma, and they’re being sued in California, right? And it’s like, they shortchange the providers and say, no, we’re not paying for this. Or it’s honestly, the patients. even that challenge back and forth between, how do I prove that it’s proving you have the condition or the need and the claim even the rights to be able to appeal.
So it’s a mess of our own making, isn’t it?
Well, the biggest problem is you and me. It’s not IT, it’s the individual patient. We don’t know. So when they write the coding and put all this stuff in, we just sort of go, Yeah, okay. Yeah, that’s good. And I hear these stories after the fact, and I was talking to somebody who said, They did the coding for their father in this way.
And then when their father came back the next time for a visit, he couldn’t get something because of the way it was coded before. And it’s like, I don’t have that. I’m not a diabetic. I’m not like, why did you code me that way? And now I can’t do this. And they’re like, well, but that’s what the doctor who saw you, that’s what he coded it.
I can’t change that now. I mean, this is, so that’s now part of your record. But we as patients. We don’t have, we’re not engaged enough and we don’t know enough, to look at it and say, Hey, I’m not a diabetic. I don’t know why you’re coding me this way. Like, my blood glucose is, actually, the average person will not be able to tell you what a diabetic’s blood glucose is or is not. We just don’t know.
It seems like, the single pair we have is Medicare, right, is that there would be, rules in place for them to evaluate and I don’t know who at Medicare is making sense out of all their data and all their claims data and what’s actually getting paid, but if I said, Okay, Medicare and Cigna and UnitedHealth, that would cover a lot of it, and say come up with some definitions of what’s acceptable.
What if it’s… left up to I don’t know, it feels like the Medicare Advantage, it’s too fuzzy, right? There aren’t rules, and even if, as I’ve been looking at it, there’s like, what is the truth here? So, if it’s, there’s so much flexibility, and you know how it is, if it’s a computer program, if you leave it where there’s all these options.
People can choose, and they’re not technically wrong.
Well, we’re going into an election year, and next year will be interesting, because, I don’t know if we’ll have the policy debates we had four years ago, or three and a half years ago, or the four years prior to that, when Obamacare was such a mainstay in the discussion, in the conversation.
But now that is sort of cemented in our vernacular, I’m not sure if we’ll have those policy things, but… I think it’s hard to argue that healthcare is changing. This article here, to me, really encapsulates the change. And actually, the last two articles, Best Buy Health and Mass General Brigham, MGB strike landmark partnership to expand healthcare at home.
That’s one of the stories. And the other is improving rural access to radiology services. Is a key topic at RS& A. Healthcare is changing. This move to at-home, remote patient monitoring, as we talked about. There’s a reason that Best Buy Health said we are a healthcare company. Best Buy said we’re a healthcare company.
The people who sell us appliances are essentially saying. No. We’re a healthcare company. And they proved it by going out and buying Current Health and a couple other of companies that offer home-based devices. And then essentially turning around and training their geek squad to go into homes.
I don’t know if they’re still going to be called geek squads, but going. Why not? Yeah. I don’t know. I mean, but essentially. Help each slot? I mean, whatever. I mean, this is a big deal. Best Buy signing a deal with Mass General Brigham, it’s like the heart of health care and a very reputable organization to deliver health care at home.
This marks a significant change by the major players to say, no, home is going to be maybe not the locus of chronic care, but it’s going to be the locus of care going forward. And we want to establish our foundation for delivering care in this format moving forward.
It makes a lot of sense, for health at home, the consumerization of healthcare… nice to have the patient involved.
And the caregivers, and we know most of the care provided in the United States is actually done at home not in the healthcare organizations as we know. But from MGB’s standpoint, this is just smart because, wow, they don’t want to deal with the hardware. They don’t want to deal with people’s homes, their home networks.
You know how it is. You’re probably tech support at home, Bill. That would be my guess. They don’t want to deal with all that, but they need all the data and they need the security and it makes for a good relationship. And it does show Best Buy’s investment in this space. and the other thing that they have a handle on is logistics.
So, I’ve got to have the right product show up at the right time, at the right house configured properly and ready for returns and all that. So, they already do that. So, they’re they’re an easy add-on. And the question is, I don’t know if Best Buy gets all the data as well.
Who gets the data, and who gets to make sense out of it is, does Best Buy get to aggregate all the data from all their devices, regardless of whether they’re working with MGB or Cleveland or Novant Health or whatever? and I talked to med device makers and the things that drive them crazy is like dealing with the the patients and their products in the home and the idea that it has to work with the phone, right?
So the idea that the patient has one remote control and it’s in their hand all the time. They’re not interested in learning your product or anything like that. It just has to come into their home and be easily turned on and configured. They don’t want to learn your UI. They don’t want to learn whatever.
They know Android or Apple and that’s it. Those are your choices, right? So from a hardware device maker. It’s actually quite challenging, inside the hospital, I can tell Health IT this is how we run, we’re GE Healthcare, whatever, you’re gonna have to learn our device because we’ve sold it in, I have thousands of them, but you take a device and put it in somebody’s home, it’s a very different thing and it’s quite challenging for the med device space to deal with, and actually industrial designers hate it, but it’s like, it’s the UI that people know, and that’s the Apple advantage.
Let me control all these devices from my phone and take, what I want to, I need to understand this data as a patient. I want it in my app, the Apple Health app, as well, right? So this is some of the challenge for the health IT folks, is like, okay, how do I influence the patient? Because the patient has to keep all this stuff running.
Not just, Geek Squad comes and sets it up and puts it on the network. But who’s going to make sure it keeps running? Patient and caregiver.
Yeah, I think it’s, I think this does mark the change. I think it’s going to be a seminal event, actually, and I think people are just looking at it like, oh yeah, MGB is doing something with Best Buy, going to the home, it’s no big deal.
Mayo is already going to the home. Others are essentially trying to do home-based services. But this to me is something that marks the start of of really changing the locus of care and expanding, the number of beds, when you measure the number of beds based on the number of beds that are within your actual building, sort of like a hotel I think that’s a mistake moving forward.
I think it’s the number of beds that are within your actual building. that you care for and that number of beds needs to include the five or six beds that happen to be in people’s homes. And in starting to think it through a little differently
It’s throughput in it. I mean, it’s throughput.
It’s not, I had five surgeries that day or 20 or 5, 000 or, whatever and it’s also, that people are spending less time in the hospital. what’s odd is that it’s less expensive to have them recover at home. Yeah, well, the best by, I’m monitoring my blood glucose. I’m sure my listeners are getting tired of hearing about this, but essentially I put this little device on and it lasts for about a week and it gives me my information as I go along.
It’s been revolutionary for me from a health perspective to see, it’s I eat this thing, it goes into my body, it impacts my body in this way. Between that, my scale, and I’m trying to think if there are any other devices that I use. I guess my phone tracks my activity and my steps and those kinds of things.
I’m probably tracking, some major items in terms of predicting my health moving forward. The question becomes, who is going to be my trusted advisor with that data? Like, if I funnel them all my data, will they be able to get back to me? And this is where I think again, we come back to AI, machine learning.
I don’t think in healthcare, we used to always think of, well, we don’t have the manpower for this. And now I think the right players are starting to think we don’t need the manpower for this. I mean, a lot of this is just, hey, I see your blood glucose is spiking. Have you considered going out for a walk?
Have you considered eating more protein and less sugar? Have you considered, it’s like these things aren’t rocket science and if you asked a doctor, they’d almost be offended. They’re just like, it’s obvious. Like a computer should be able to spit out a message to let you know that and that’s true.
That’s exactly what AI machine learning could do or any algorithms for that matter. We just need to start thinking about it a little different and say no, it’s every bed in our community that we want to be caring for. And if you have health information, send it to us, and we will be your trusted advisor and help you make meaning of it.
Because if we don’t, somebody else will. Yeah, I mean, and for these devices, because you could build a model that took all these devices, these common consumer devices as input. So, Dexcom, Oura Ring. Withings scale, a couple, of things that are real-time or near real-time. You could have batch input of blood pressure.
Other things, also just regular survey data, and that’s the basics of RPM already, and so a lot of us are doing RPM just on our own, but we don’t, we have to go to these kind of proprietary, I got a customer portal here, and there, and I’m like, I don’t want all those, I just want one, it’s mine.
And multiple devices can enter into it, no one can own that whole ecosystem and it’s gonna, and I think this is some of the challenge health IT has because it’s going to be different devices, and it’s different physiological data. That you want, and a different model because based on age and population and weight and all these other things, but you can see there’s some similarities, and for a population that’s common, some of it’s like, just, we wear the sensor, do you want to know better? Do you want to be informed or influenced? But big parts of America don’t want to know. It’s a lot just to step on the scale. I think this is a lot of the health, the hospital organizations are dealing with, part of the population that’s In denial, right?
So they want to be rescued at, after a life of living really hard and not really caring maybe that much, a, that’s not a way to live a long quality life, unfortunately.
Yep. So I’m looking at Best Buy stock has jumped 6 percent in the last 30 days.
I think that’s an indication of what people think of this. If they can figure out a way to get per member per month kind of rates, if Best Buy can figure out how to tap into that on a national scale with partners like MGB and, obviously there’s big players out there still to be to consider this and move forward.
And I think your point of not reinventing the wheel and trying to understand how to deliver services in the home, not trying to understand, I mean, they come into our home right now and they install a sound system where they install a TV and that kind of stuff. we take for granted how complex that is to send a person that is employed by you into somebody’s home and to, do that work.
There’s liability associated with that. There’s complexity associated with that. and I can’t rattle off five companies that can do that.
I know, I think about Comcast. I mean, you think of Like Amazon doesn’t necessarily have that ability either. It has all the logistics, but not the kind of in-home, which is unusual.
And dealing with people in their homes. I mean, in their Wi-Fi, it’s, No one knows how anything works,
Bill. I know. That’s wild. They can’t remember their passwords.
None of that. Well, I’m looking forward to the day when we do not have passwords. I don’t know how we’re going to get there, but… I used to think it was gonna be by voice and it’s not gonna be by voice. ’cause they could replicate that.
I have no idea what it’s gonna be. Blood, maybe it’s gotta, might be blood.
Oh my gosh. Anything’s gotta be better than at last count I’m well up over 200 passwords because they don’t want you to reuse it on every site you go to. But still, it’s like, my methodology, look, if they cracked my methodology, they could figure out half my passwords. because I have to remember them. I can’t just have 200 out there. There’s got to be somebody, anybody, come to our rescue on this one. It would be great. I only have one password, so, I no longer dream them up.
No, yeah, it gets hard. Bob, I want to thank you I want to thank you for your time. As always, really enjoy our conversations. Thank you.
Me too, Bill. Thanks so much for your time. Appreciate it.
And that is the news. If I were a CIO today, I think what I would do is I’d have every team member listening to a show just like this one, and trying to have conversations with them after the show about what they’ve learned.
And what we can apply to our health system. If you wanna support this week Health, one of the ways you can do that is you can recommend our channels to a peer or to one of your staff members. We have two channels this week, health Newsroom, and this week Health Conference. You can check them out anywhere you listen to podcasts, which is a lot of places apple, Google, , overcast, Spotify, you name it, you could find it there. You could also find us on. And of course you could go to our website http://thisweekhealth.com, and we want to thank our new state partners again, a lot of ’em, and we appreciate their participation in this show.
Cedar Sinai Accelerator Clearsense, CrowdStrike, Digital Scientists, optimum, Pure Storage, Suretest, tausight, Lumeon, and VMware who have invested in our mission to develop the next generation of health leaders. Thanks for listening. That’s all for now.