AI that reviews patients 50X faster than manual audit—with 90%+ accuracy.
CommuniCare Health Services needed to close the gap between clinical documentation and coded diagnoses across 20,000+ Medicare Advantage patients in 7 states. We built an AI engine that analyzes six clinical data sources to surface missed HCC codes—turning 1-hour manual chart reviews into 60-second AI-assisted audits.
RAF Score Improvements
Diagnosis Accuracy
Patients Served
Faster Patient Review
Closing the documentation-to-coding gap at scale.
In Medicare Advantage, Risk Adjustment Factor (RAF) scores determine reimbursement rates. Missed Hierarchical Condition Category (HCC) codes mean missed revenue—and inaccurate patient risk profiles that affect care planning. CommuniCare Health Services, one of the nation's largest post-acute care providers, had a problem at scale: diagnoses documented in clinical notes weren't making it to claims.
Digital Scientists built an AI-powered coding engine that ingests data from six clinical sources—diagnoses, health risk assessments, medications, progress notes, lab results, and claims—to identify missed ICD-10 codes with confidence scoring and clinical evidence linking. The platform reviews each patient in roughly 60 seconds, compared to the hour-long manual audits it replaced.
The engine composition is 79% SQL-driven queries against structured clinical data, 20% generative AI analysis using GPT-4, and 1% DBSCAN clustering for pattern detection. Every recommendation links directly to supporting documentation—audit-defensible from day one.
Millions in missed risk adjustment from incomplete coding.
CommuniCare's providers were documenting conditions in clinical notes, but those diagnoses weren't consistently being captured as coded claims. With 20,000+ patients across 7 states and 245 providers, there was no systematic way to ensure HCC codes matched what was documented in the chart.
The gap wasn't competence—it was capacity. Manual chart audits took roughly an hour per patient. Chronic conditions from prior years weren't being recaptured annually. And every uncoded diagnosis created audit exposure on top of lost revenue.
Before Digital Scientists
1 hour per patient audit
Manual review of clinical documentation, medications, lab results, claims history
Documentation-to-coding gap
Diagnoses in notes not making it to claims—HCC codes left on the table
Chronic condition recapture failure
HCCs from prior years not being recaptured annually as CMS requires
Audit exposure at scale
Coding without clear documentation linkage across 20K+ patients and 7 states
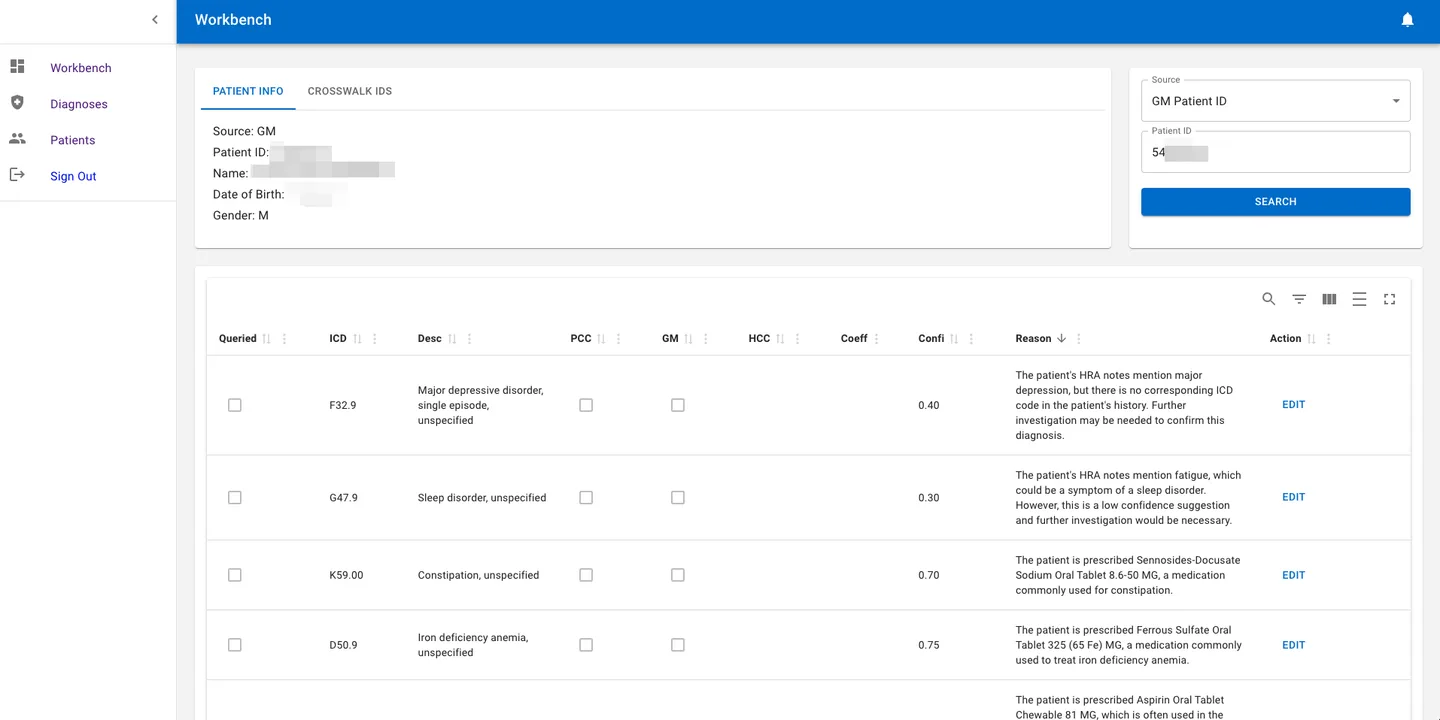
An AI engine that reviews patients in 60 seconds.
The platform analyzes six clinical data sources per patient to surface missed ICD-10 codes, each with a confidence score and direct link to supporting documentation. Coders review, accept, or modify—never black-box automation.
AI Diagnosis Engine
Ingests diagnoses, health risk assessments, medications, progress notes, lab results, and claims data. Identifies missed ICD-10 codes by comparing documented conditions against what's been coded.
- Confidence scoring per recommendation
- Prior-year HCC recapture identification
- Clinical evidence linking for every code
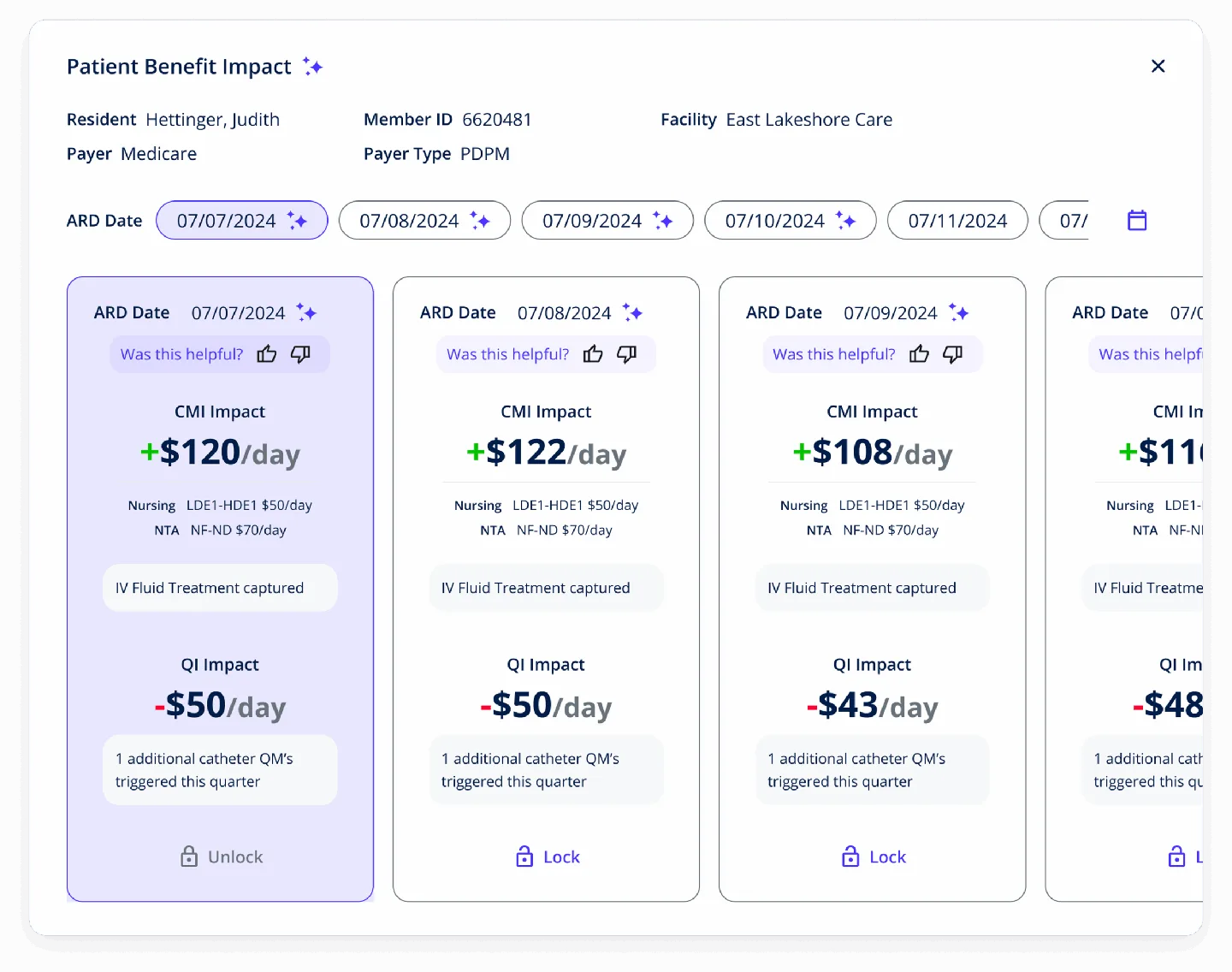
Coder Workbench
Purpose-built interface for medical coders. Each patient shows AI-suggested ICD codes with confidence scores, plain-language reasons derived from clinical notes, and one-click edit actions.
- Patient info + crosswalk IDS in one view
- AI reasons explain why each code was suggested
- HCC, coefficient, and comorbidity data per code
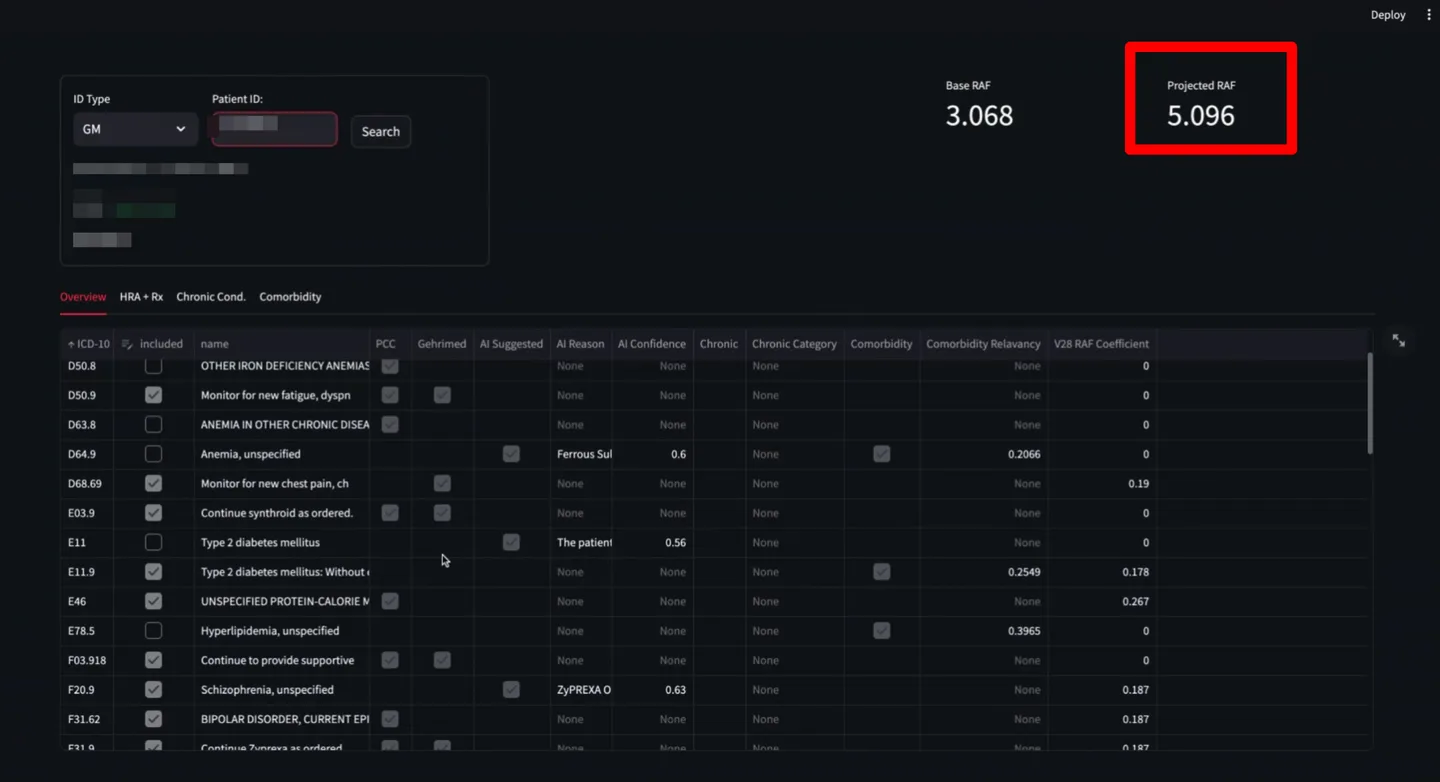
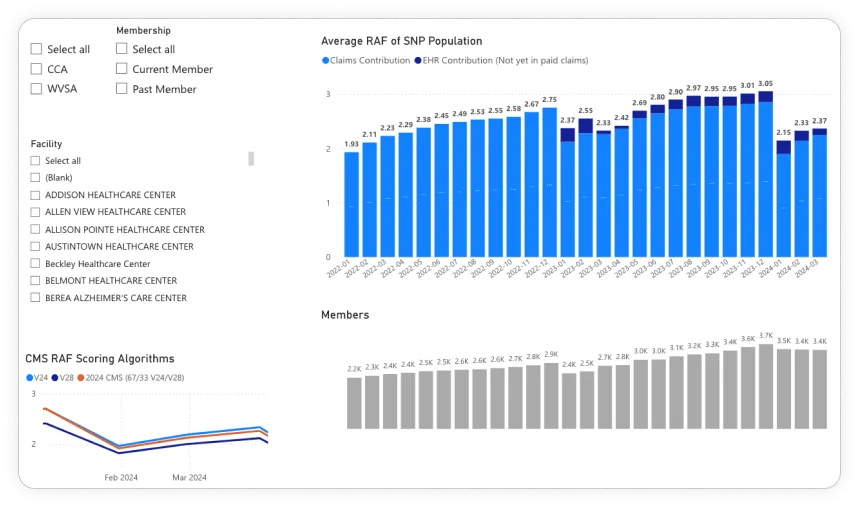
RAF Score Analytics
Real-time RAF calculation showing base vs. projected scores per patient. The dashboard breaks down each ICD code's contribution to the RAF score with HCC category, coefficient, and comorbidity multipliers.
- Base vs. projected RAF side by side
- ICD-to-HCC coefficient mapping
- Facility-level and provider-level comparisons
Six data sources. Four AI models. One prioritized recommendation list.
The engine pulls from every relevant clinical data source available for each patient, runs four parallel analysis models, and produces a ranked list of missed ICD-10 codes—each with a confidence score and audit-ready evidence chain.
Data Sources
Diagnoses
ICD-10 codes
Health Risk Assessments
HRA records
Medications
Rx data
Progress Notes
Clinical narratives
Lab Results
Diagnostic labs
Claims Data
Prior-year claims
AI Models
DBSCAN Clustering
Unsupervised clustering (eps=0.62, k=7) identifies patient cohorts with similar clinical profiles but different coding patterns—surfacing systematic gaps.
GPT-4 Analysis
Generative AI reviews clinical narratives to identify implied diagnoses—conditions described but not explicitly coded. Provides plain-language reasoning for each suggestion.
NLP Notes Mining
Natural language processing extracts structured clinical signals from unstructured progress notes, identifying conditions referenced in free-text documentation.
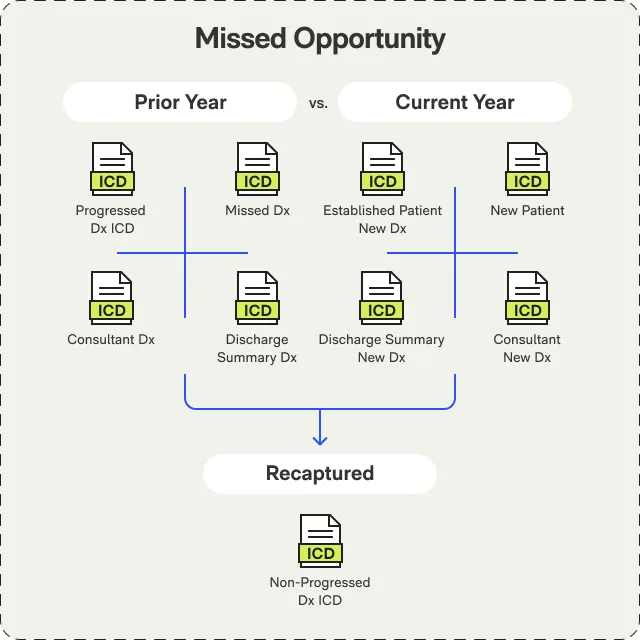
Claims Gap Analysis
Compares current-year coded claims against prior-year HCC history to identify chronic conditions that should be recaptured annually per CMS requirements.
Per-patient review time (vs. ~1 hour manual)
Of patients had additional valid ICD-10 codes identified
Average RAF score increase per impacted patient
Two phases. Data foundation first, then AI.
We didn't start with the AI model. We started with the data—building a secure pipeline from CommuniCare's on-premise MSSQL databases to our AWS environment via VPN tunnel, then validating data quality before training began.
Aug – Nov 2023
Data Pipeline & Model Development
- Secure VPN tunnel from on-premise MSSQL to AWS
- 7 tables across 3 databases mapped and normalized
- DBSCAN clustering and GPT-4 model training
- HIPAA and CMS RAPS compliance validation
Nov 2023 – Present
Platform Build & Production Deployment
- React/TypeScript frontend with Material UI coder workbench
- Python/FastAPI backend on AWS Kubernetes (EKS)
- Gehrimed, PointClickCare, and Acclivity EHR integrations
- Rollout across 7 states, 245 providers, 20K+ patients
$10M+ in RAF improvements. $2K+ per impacted patient per year.
These numbers come from actual RAF score improvements tracked across CommuniCare's Medicare Advantage population. Roughly 40% of patients reviewed had additional valid ICD-10 codes identified by the engine.
Financial Impact
Annualized revenue impact from more accurate risk adjustment coding.
Additional annual reimbursement per impacted patient from corrected RAF scores.
Mean RAF score improvement per impacted patient—from codes the engine identified that manual review missed.
Operational Impact
60-second AI-assisted audit vs. ~1 hour manual chart review per patient.
Of patients reviewed had additional valid ICD-10 codes identified by the AI engine.
AI recommendations validated against clinical documentation with high accuracy.
Wrapped around existing EHR systems.
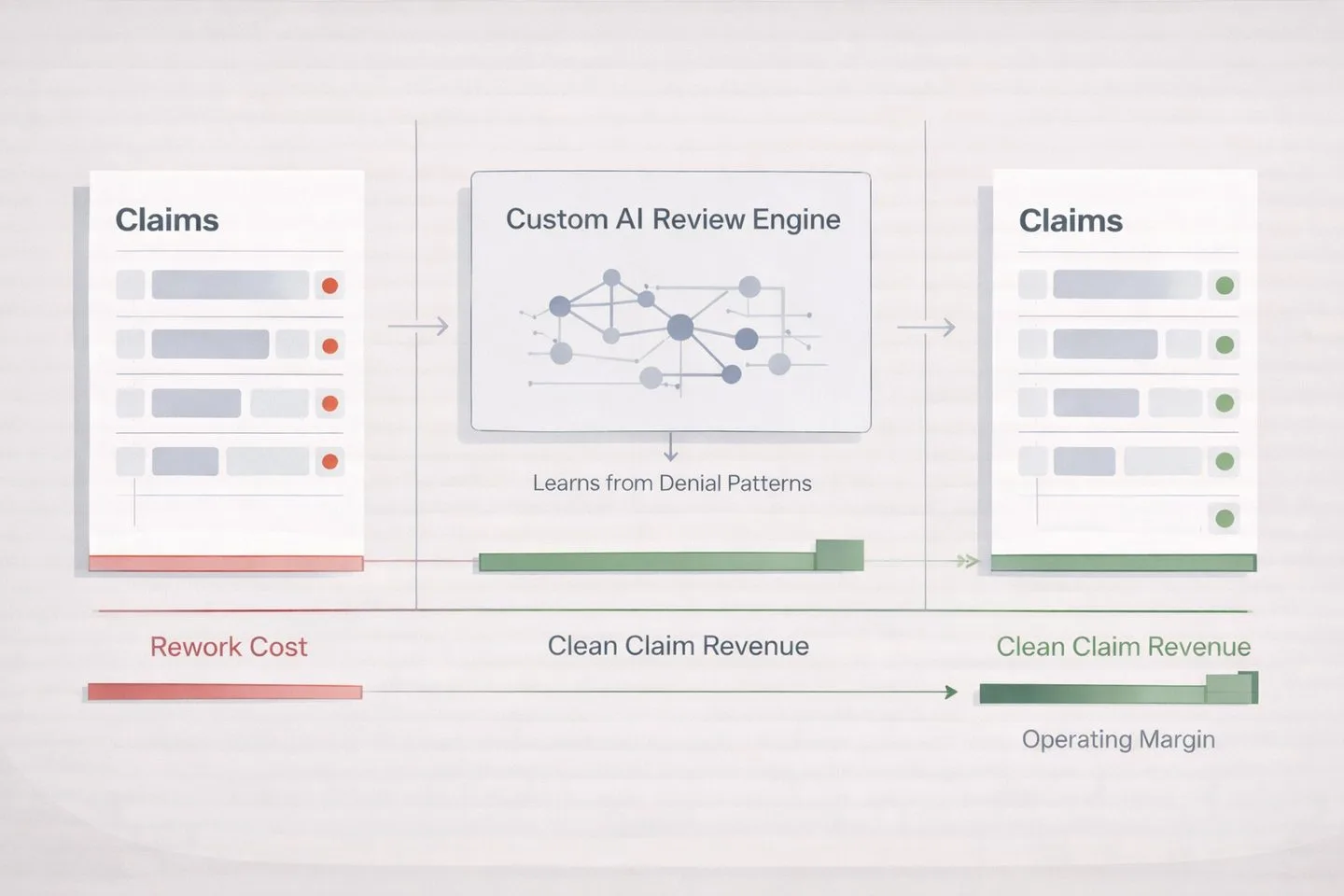
No rip-and-replace. The platform integrates directly with CommuniCare's existing EHR ecosystem, pulling clinical data for analysis and surfacing recommendations within the coder's workflow. No separate login, no duplicate data entry.
Production Integrations



Standards & Compliance
HIPAA Compliant
End-to-end encryption, VPN tunnel to on-premise data, AWS HIPAA-eligible services
CMS RAPS Compliance
Coding recommendations align with CMS Risk Adjustment Processing System requirements
Audit-Defensible
Every recommendation linked to clinical documentation with full evidence chain
Gated Learning
Deliberate, validated model improvements—not automated retraining. Every update reviewed before deployment.
Responsible AI, not black-box automation.
Healthcare AI fails when it's treated as a black box. This platform was built for explainability, auditability, and human oversight at every step.
79% structured queries, 20% AI
Most of the engine runs on deterministic SQL queries against structured clinical data. Generative AI handles the hard part—unstructured notes and implied diagnoses—but it's 20% of the workload, not 100%. This makes the system explainable and predictable.
Every code is audit-defensible
Each AI recommendation links directly to the clinical documentation that supports it. When auditors ask "why was this coded?"—the evidence chain is one click away. No unsupported codes. No guessing.
Gated learning, not continuous
The model doesn't retrain itself automatically. Improvements are deliberate and validated—every update reviewed by clinical and engineering teams before production deployment. This prevents drift and ensures consistency.
What's your risk adjustment opportunity?
If missed HCC codes are costing you millions in RAF revenue, let's talk. 30-minute call to assess your opportunity.
Schedule Assessment CallRelated Insights
From Our Blog

Leveraging AI tools in Social Need Screening and Intervention – comments on proposed changes to HEDIS SNS-E measure
Feb 19, 2025

AI & The Job Landscape, ChatGPT’s Role, & The Future of RPM
Dec 12, 2023
Leveraging AI for ROI in Healthcare: 10 Custom Solutions for 2026
Nov 28, 2025